The Real Deal About Dentures, Dental Implants, and Taking Care of Your Teeth
The Real Deal About Dentures, Dental Implants, and Taking Care of Your Teeth
You know what nobody tells you? Losing teeth changes everything. Not just your smile—though that's part of it—but how you experience food, how you talk to people, even how you feel when you look in the mirror. And when you start looking into solutions, suddenly you're drowning in options: traditional dentures, dental implants, implant-supported dentures, and a dozen variations of each. Then there's the whole question of how to actually take care of whatever you end up with.
I'm going to walk you through all of it, not with the sanitized version your dentist's brochure gives you, but the real story. What actually works, what doesn't, what costs what, and how to keep your mouth healthy whether you've got all your natural teeth or you're working with replacements. This isn't about scaring you or selling you on one solution over another. It's about giving you enough straight talk that you can make a decision you'll still feel good about five years from now.
Why Dental Care Matters More Than You Think
Before we get into dentures and implants, let's talk about why any of this matters in the first place. Your mouth is basically the gateway to your entire body. Everything you eat passes through it. Infections in your mouth don't just stay in your mouth—they can affect your heart, your blood sugar if you're diabetic, even your risk of stroke. This isn't scare tactics; this is just biology.
When you've got healthy teeth and gums, taking care of them is pretty straightforward: brush twice a day, floss once (yeah, I know you don't, but you should), see your dentist twice a year for cleanings. That routine prevents most problems before they start. Cavities, gum disease, tooth loss—these things don't usually happen overnight. They're the result of months or years of bacteria doing their thing while you ignore the warning signs.
But here's what gets interesting: good dental care isn't just about preventing problems. It's about maintaining your quality of life. Being able to eat what you want without pain or difficulty matters. Speaking clearly matters. Smiling without feeling self-conscious matters. These aren't superficial concerns—they affect your mental health, your social connections, your career opportunities, and your overall happiness.
When teeth start failing or disappearing altogether, suddenly dentalcare becomes way more complicated. You're not just brushing and flossing anymore. You're figuring out adhesives, special cleaning solutions, wondering if you need surgery, calculating whether you can afford treatment, and trying to understand dental jargon that might as well be a foreign language.
The stakes feel higher because they are higher. Once a tooth is gone, it's gone. Your options at that point are all about replacement and damage control, not restoration. So everything you do to maintain your natural teeth—even the ones that aren't perfect—is worth the effort.
Understanding Traditional Dentures: The Full Picture
Let's start with dentures because they're the option most people have at least heard of. Your grandparents probably had them. Maybe your parents do. They've been around forever, and modern versions are light-years better than the clunky things people wore fifty years ago.
Traditional dentures are removable prosthetic teeth. Full dentures replace all your teeth in an arch (upper, lower, or both). Partial dentures fill in gaps when you're missing some teeth but still have others worth keeping. They're made from acrylic resin for the gum-colored base, with teeth that are either acrylic or porcelain. High-quality dentures can look incredibly natural—most people won't realize you're wearing them unless you tell them.
The mechanics are simple: upper dentures create suction against your palate, while lower dentures rest on your gums and are held in place by your tongue and cheeks (with help from adhesives). Partial dentures use metal clasps or precision attachments to hook onto your remaining natural teeth.
Now, here's what the brochures emphasize: dentures are affordable, non-surgical, and they restore your ability to eat and speak. All of that's true. What they often downplay is that dentures come with a learning curve and some genuine limitations.
When you first get dentures, they feel weird. Really weird. There's this foreign object in your mouth, and your brain is not happy about it. You'll produce extra saliva for the first few days. You might gag, especially with upper dentures that cover your palate. Speaking feels different—certain sounds come out wrong until you retrain your tongue to work around the dentures. Eating is an adventure; you've got to relearn how to chew because the dentures don't give you the same sensory feedback your natural teeth did.
Most people adapt within a few weeks, but "adapt" is the key word. You get used to it, but it never feels exactly like having your own teeth. Dentures can slip at inopportune moments—while you're laughing, coughing, or eating certain foods. This creates anxiety. You become hyperaware of your teeth in social situations, constantly checking with your tongue to make sure everything's still in place.
The food restrictions are real. Sticky stuff like caramel or peanut butter can pull your dentures loose. Hard foods can be uncomfortable or even painful. Chewy meats are difficult. Corn on the cob, raw apples, crusty bread—these go from everyday foods to calculated risks. Some people adjust fine and eat almost normally. Others find their diet genuinely limited.
Then there's the nightly routine. Dentures come out for cleaning and to give your gums a rest. You scrub them with a denture brush and special cleanser, soak them overnight (or at least for several hours), and pop them back in the next morning. For some people, this is no big deal. For others, it's a depressing nightly reminder that these aren't their real teeth. It also complicates spontaneous overnight trips—you need your cleaning kit, your soaking container, the whole setup.
Dentures need maintenance. They don't fit perfectly forever because your gums and bone change shape over time. You'll need periodic adjustments, relines (where they resurface the base to match your current gum contours), and eventually complete replacement. Figure on dentures lasting five to eight years before needing to be remade.
The bone loss issue is significant. When you lose teeth, your jawbone in those areas starts to shrink because it's no longer getting the stimulation from chewing. Dentures don't stop this process—in fact, because they put pressure on your gums, they can actually accelerate bone loss. Over years, this changes your facial structure. Your face can take on that sunken look you associate with elderly people, your lips lose support, wrinkles deepen around your mouth. It ages you.
But despite all these drawbacks, dentures work for millions of people. They're accessible—most people can afford them. They're non-invasive—no surgery required. They're quick—you can have them within a few weeks of losing your teeth. And they're removable, which some people actually prefer. If you've got health issues that preclude surgery, or if cost is a major barrier, or if you're just not interested in implants, dentures are a legitimate solution.

Dental Implants: The Permanent Alternative
Now let's talk about the other end of the spectrum: dental implants. These have become the gold standard for tooth replacement, and once you understand how they work, you'll see why.
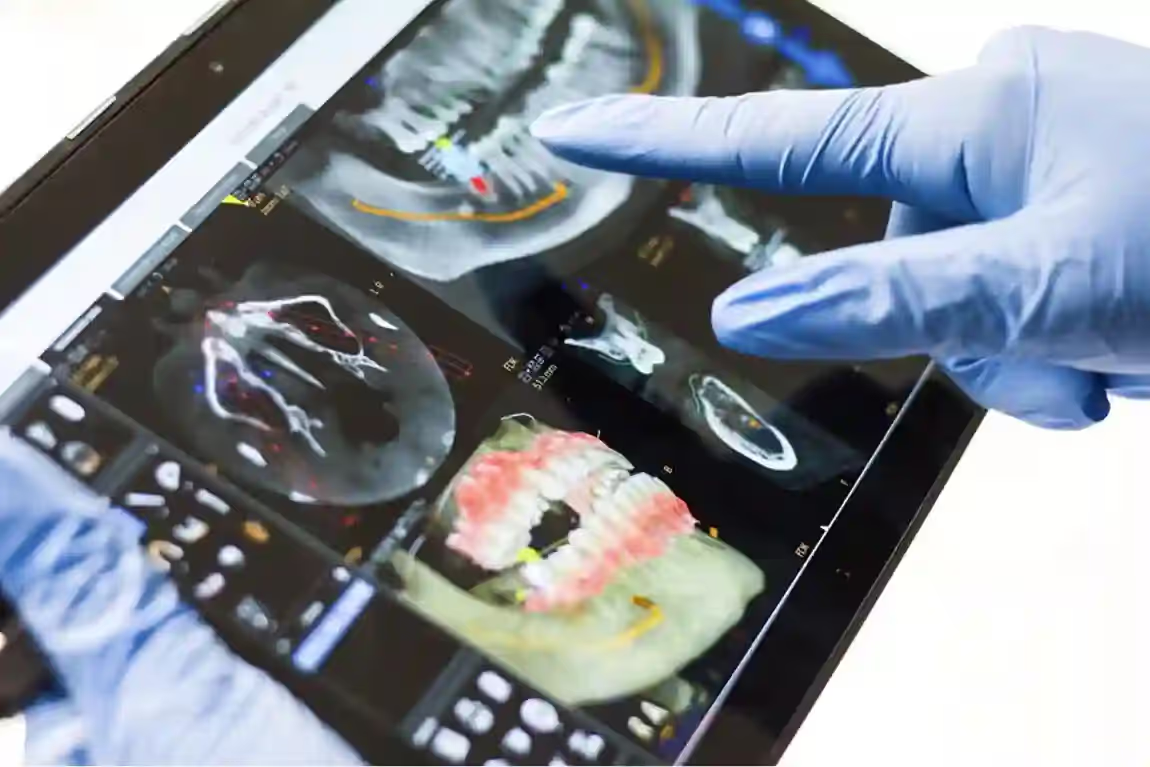
A dental implant is essentially an artificial tooth root. It's a titanium post—usually shaped like a screw—that a surgeon places directly into your jawbone where your natural tooth root used to be. Over the next few months, something remarkable happens: your bone grows around the implant and fuses with it through a process called osseointegration. The titanium literally becomes part of your jawbone.
Once that integration is complete, the dentist attaches an abutment (a connector piece) to the top of the implant. This sticks up through your gum tissue. Finally, they mount a crown—the tooth-shaped cap that everyone sees—onto the abutment. The whole assembly replaces everything you lost: root, structure, and visible tooth.
The result functions almost identically to a natural tooth. You can bite with normal force. You can eat anything—apples, steak, corn on the cob, whatever. The implant doesn't move or slip because it's anchored in bone. You brush and floss it like a regular tooth. Most people forget it's not their original tooth within weeks.
The benefits extend beyond function. Implants preserve your bone because they stimulate it just like natural tooth roots do when you chew. This maintains your facial structure and prevents that aged, sunken appearance. They don't require modification of adjacent teeth—a big advantage over bridges, which require grinding down healthy neighboring teeth to serve as anchors. And they last. We're talking decades, often a lifetime, if you take reasonable care of them.
The titanium post itself is incredibly durable. It doesn't decay, doesn't get cavities, and rarely fails once it's integrated. The crown might need replacement after fifteen or twenty years of hard use—crowns can chip or wear down—but replacing just the crown is straightforward. The implant itself typically stays put forever.
Of course, implants aren't perfect for everyone. They require surgery, which means healing time and all the risks that come with any surgical procedure (infection, nerve damage, sinus problems for upper teeth, though these complications are rare with experienced surgeons). The process takes months from start to finish—you need time for the implant to integrate before you can put a crown on it.
Cost is the big barrier for most people. A single implant, including the post, abutment, and crown, runs $3,000 to $6,000. Multiple implants multiply that cost quickly. Replace a whole mouth and you're looking at $50,000 to $100,000 or more. Yes, they last longer than other options, and yes, the math works out better over decades, but that initial investment is steep.
Not everyone qualifies medically. You need adequate bone density, and if you've been missing teeth for years, you might need bone grafting first. Active gum disease has to be treated before implant placement. Certain health conditions—uncontrolled diabetes, active cancer treatment, some autoimmune disorders—complicate things. Heavy smoking dramatically increases failure rates. So does teeth grinding if you don't wear a night guard.
But for people who do qualify and can manage the cost, implants deliver results that other options simply can't match. The satisfaction rate is north of 95%. Most people who get implants say they'd do it again without hesitation and that it significantly improved their quality of life.
The Sweet Spot: Implant-Supported Dentures
Here's where things get really interesting, because you don't have to choose between traditional dentures and full implant restoration. There's a middle option that combines the best aspects of both: implant-supported dentures (sometimes called implant-retained dentures or overdentures).
The concept is elegant. Instead of replacing every tooth with individual implants, the surgeon places four to six implants per arch. These serve as anchors for a denture that either snaps onto them (removable type) or gets screwed permanently into place (fixed type). You get the stability and bone preservation of implants without the cost and complexity of replacing every single tooth.
The difference in stability is night and day compared to traditional dentures. With regular dentures, you're working with maybe 25% of natural bite force because there's only so much pressure your gums can handle. With implant-supported dentures, you're back to 70-80% of natural bite force. This means you can actually eat normally again—steak, raw vegetables, crusty bread, all the stuff that was problematic with traditional dentures.
The denture doesn't move. Ever. No slipping while you talk, no awkward moments while eating, no constant anxiety about whether your teeth are going to shift. You speak normally, you smile confidently, you forget you're wearing dentures most of the time.
There are two main varieties. The removable version snaps onto the implants using special attachments—you can take it out for cleaning, which some people prefer. The fixed version (often marketed as All-on-4 or All-on-6, depending on how many implants) is permanently attached. Only your dentist can remove it, and you treat it exactly like natural teeth—brushing, flossing around the implants, and forgetting it's there. Most people prefer the fixed type because it feels more like having real teeth, but removable has its fans too.
The upper denture design is particularly clever. With traditional dentures, the upper plate covers your entire palate, which affects how food tastes and can trigger gagging. Implant-supported upper dentures don't need that full palate coverage because the implants provide retention. Your palate stays open, food tastes better, and there's no gagging issue.
Cost-wise, you're looking at something between traditional dentures and full implant restoration—maybe $15,000 to $35,000 per arch, depending on your location and the specifics of your case. That's not pocket change, but it's dramatically less than $80,000 for a full mouth of individual implants while delivering many of the same benefits.
The timeline is faster too. With the All-on-4 technique, many dentists can give you temporary teeth the same day as your implant surgery. You walk in with failing teeth or traditional dentures, and you leave with a functional smile attached to new implants. The temporary teeth stay in place while you heal (several months), then you get the permanent dentures made.
This option works particularly well for people who've been wearing traditional dentures and want an upgrade without going full implant restoration. It's also great for folks who've lost most or all of their teeth in one or both arches and want something stable that won't break the bank.
Comparing Your Options: Real Talk
Let's lay out the practical differences because that's what actually helps you make a decision.
Traditional Dentures:
- Cost: $1,000 to $3,000 per arch
- Timeline: Few weeks from impressions to final dentures
- Surgery: None
- Function: Limited bite force (about 25% of natural), some food restrictions
- Stability: Can slip or move, especially lower dentures
- Maintenance: Remove nightly for cleaning, periodic adjustments needed, replacement every 5-8 years
- Bone preservation: None—actually accelerates bone loss
- Comfort: Takes getting used to, never feels exactly like natural teeth
- Best for: People who can't afford implants, aren't candidates for surgery, or prefer non-invasive options
Dental Implants (Individual):
- Cost: $3,000-$6,000 per tooth
- Timeline: 6-9 months per implant (including healing)
- Surgery: Yes—separate procedure for each implant
- Function: Virtually identical to natural teeth
- Stability: Completely stable—doesn't move at all
- Maintenance: Brush and floss like natural teeth, regular dental cleanings
- Bone preservation: Excellent—maintains bone density
- Comfort: Feels like natural teeth within weeks
- Best for: Replacing one to several teeth when you want the most durable, natural-feeling solution and can afford it
Implant-Supported Dentures:
- Cost: $15,000-$35,000 per arch
- Timeline: 3-6 months from surgery to final dentures
- Surgery: Yes—placing 4-6 implants per arch
- Function: Near-normal bite force (70-80% of natural), minimal food restrictions
- Stability: Completely stable—no movement or slipping
- Maintenance: Fixed type: brush and floss like natural teeth; Removable type: remove for cleaning
- Bone preservation: Good—implants stimulate bone at anchor points
- Comfort: Feels natural after initial adjustment period
- Best for: People missing most or all teeth in an arch who want stability and function without the cost of full implant restoration
The choice often comes down to three factors: budget, medical candidacy, and personal priorities. If money is tight and surgery isn't an option, traditional dentures might be your answer. If you want the absolute best function and longevity regardless of cost, individual implants deliver. If you want excellent stability and function at a more manageable price point, implant-supported dentures might be your sweet spot.
Dental Care with Natural Teeth: Building a Foundation
Whether you've still got all your natural teeth, you're missing a few, or you're thinking about the future, maintaining what you have is priority number one. Every tooth you keep is one you don't have to replace. And good dental care habits now make any future dental work easier, cheaper, and more successful.
The basics haven't changed since you were a kid: brush twice a day, floss daily, see your dentist every six months. But let's talk about doing these things effectively, not just going through the motions.
Brushing technique matters more than you'd think. You want a soft-bristled brush (hard bristles damage your gums and enamel) held at a 45-degree angle to your gum line. Make small circular motions, spending about 30 seconds on each quadrant of your mouth for a total of two minutes. Electric toothbrushes make this easier—many have built-in timers, and the oscillating action cleans more effectively than manual brushing for most people.
The toothpaste matters less than you think. Any fluoride toothpaste is fine. Don't fall for gimmicks. Whitening toothpastes are mostly hype—they're slightly abrasive, which removes surface stains but doesn't actually change your tooth color and can damage enamel with overuse. Sensitivity toothpastes with potassium nitrate actually work for sensitive teeth, though they take a few weeks. Otherwise, pick something you like the taste of so you'll actually use it.
Flossing is where most people fail. I get it—it's annoying, it makes your gums bleed (at first), and it feels like you're adding five minutes to your routine. But here's the thing: brushing only cleans about 60% of your tooth surfaces. The other 40% is between your teeth where the brush can't reach. Skip flossing, and you're leaving that 40% to rot.
If traditional floss is too much hassle, use floss picks, interdental brushes, or a water flosser. Water flossers (like Waterpik) are genuinely effective and easier for people with dexterity issues, braces, or implants. They're not quite as good as traditional floss for removing plaque, but they're way better than not flossing at all.
Mouthwash is optional for most people. It freshens breath and can reduce bacteria, but it doesn't replace brushing and flossing. If you're prone to cavities, a fluoride rinse helps. If you've got gum disease, your dentist might recommend an antimicrobial rinse like chlorhexidine. Otherwise, it's personal preference.
Diet affects your teeth more than most people realize. Sugar is the obvious villain—bacteria in your mouth convert it to acid, which dissolves enamel. But frequency matters more than quantity. Sipping a sugary drink all day is worse than drinking it all at once because your teeth are under constant acid attack. Same with snacking constantly versus eating three meals.
Acidic foods and drinks (citrus, soda, wine, sports drinks) erode enamel directly—you're basically bathing your teeth in acid. If you're going to consume them, do it with meals rather than sipping throughout the day, and rinse your mouth with water afterward. Don't brush immediately after acidic foods; you'll scrub the softened enamel away. Wait at least 30 minutes.
Water is your friend, especially if it's fluoridated. Drinking water throughout the day rinses away food particles and bacteria, keeps your mouth from getting too dry, and delivers fluoride to your teeth. If you have well water, consider a fluoride supplement—it genuinely reduces cavities, despite what the conspiracy theorists claim.
Your dentist visits aren't just about cleaning—they're about catching problems early. A small cavity is a simple filling. That same cavity, left untreated, becomes a root canal or extraction. Gum disease caught early is reversible with better brushing and flossing. Advanced gum disease requires surgery and can cost you teeth. The six-month checkup interval exists for good reasons.
Dental Care with Dentures: What Actually Works
If you're wearing dentures or about to get them, your dentalcare routine changes significantly. Dentures need different care than natural teeth because they're different materials with different vulnerabilities.
First rule: take them out at night. Your gums need a break from the constant pressure. Leaving dentures in 24/7 increases your risk of fungal infections, accelerates bone loss, and contributes to bacterial buildup. Give your mouth at least six to eight hours of denture-free time, typically overnight.
Cleaning dentures properly prevents staining, odor, and bacterial growth. Rinse them after eating to remove loose food particles. Once daily—usually before bed—give them a thorough cleaning with a denture brush and denture cleanser. Regular toothpaste is too abrasive for dentures; it scratches the surface, which creates places for bacteria to hide and makes staining worse.
Hold dentures over a folded towel or a sink filled with water while cleaning them. They're more fragile than you'd think, and dropping them on a hard surface can crack or break them. Use cool or lukewarm water, not hot—heat can warp the material.
Soak dentures overnight in a denture-cleaning solution or plain water. This keeps them from drying out and warping. There are various soaking solutions available—effervescent tablets, antimicrobial soaks, etc. They all work fine. Some people use a mild vinegar solution (one part white vinegar to ten parts water) as a budget option for removing mineral buildup.
Your gums still need attention even though you don't have natural teeth. Brush your gums, tongue, and palate with a soft brush before putting your dentures back in. This stimulates circulation, removes bacteria, and keeps your mouth healthier. If you've got remaining natural teeth that the partial dentures clasp onto, those need extra-careful brushing and flossing—they're at higher risk for decay and gum disease.
Check your dentures regularly for signs of wear. Look for cracks, chips, loose teeth, or rough spots that might irritate your gums. Small problems are easier and cheaper to fix than major damage. If your dentures feel loose or uncomfortable, don't try to adjust them yourself with super glue or other DIY fixes. See your dentist for a proper reline or adjustment.
Denture adhesive can help with stability, especially for lower dentures, but shouldn't be necessary if your dentures fit properly. If you're using massive amounts of adhesive to keep your dentures in place, they probably need adjustment or relining. A thin layer of adhesive is fine for extra security in social situations, but you shouldn't depend on it for everyday wear.
Watch for signs of problems: persistent sore spots on your gums, white patches in your mouth (could be thrush), difficulty chewing or speaking, dentures that feel increasingly loose. These all warrant a dentist visit. Don't tough it out hoping things will improve—they usually won't without intervention.
Your diet matters with dentures, not just for the practical reasons we discussed earlier (avoiding foods that pull dentures loose or cause discomfort) but for nutrition. If you're avoiding meat, raw vegetables, and other nutritious foods because they're hard to eat with dentures, you might end up with nutritional deficiencies. Work with your dentist to maximize your dentures' functionality, and consider whether implant-supported options might give you more dietary freedom.
Dental Care with Implants: Simpler Than You'd Think
Here's the good news: caring for dental implants is almost identical to caring for natural teeth. Almost. There are a few specifics worth knowing, but mostly it's just applying the same good habits.
Brush twice daily with a soft-bristled brush, just like you would with natural teeth. Pay particular attention to where the crown meets your gum—plaque accumulates there, and inflammation can develop if you're not thorough. Electric toothbrushes work great and aren't too aggressive for implants. Some dentists recommend low-abrasion toothpaste around implants, but any standard fluoride toothpaste is fine for most people.
Flossing around implants is non-negotiable. Use regular floss, floss threaders, or a water flosser—whatever you'll actually use consistently. The goal is to clean that area where the abutment comes through your gum. Bacteria and plaque can accumulate there and cause peri-implantitis (inflammation around the implant), which can lead to bone loss and implant failure if left untreated.
Some people like interdental brushes for cleaning around implants. These tiny brushes get into spaces that floss might miss. They're particularly useful if you've got implant-supported bridges where multiple crowns are connected.
Water flossers deserve special mention for implant care. They're effective at flushing out bacteria from around the abutment, and many people find them easier to use than traditional floss, especially around the back teeth. If a water flosser means you'll actually clean around your implants daily instead of skipping it half the time, it's worth the investment.
Regular dental visits every six months are crucial—maybe even more so than with natural teeth. Your hygienist will clean around your implants using specialized tools (not the same scalers used on natural teeth, which can scratch the implant surface). Your dentist will check the implant, the surrounding bone, and the crown for any issues. These checkups catch potential problems early.
Avoid habits that damage natural teeth because they'll damage implants too. Don't chew ice, don't use your teeth to open packages, don't bite your nails. If you grind your teeth at night, wear the night guard your dentist makes you. Grinding can crack the crown, damage the abutment connection, or even fracture the implant itself over time.
Smoking remains problematic even after your implants have healed. It doesn't just affect initial healing—it increases your long-term risk of peri-implantitis and implant failure. The reduced blood flow compromises your body's ability to fight infection around the implant. If you smoke, quitting provides benefits that extend far beyond your dental health.
Watch for warning signs: redness, swelling, or bleeding around the implant; any sense that the implant feels loose; pain or discomfort; pus or discharge. These could indicate peri-implantitis or other problems that need professional attention. The sooner you address issues, the better the outcome.
The crown might need replacement eventually, typically after fifteen to twenty-five years depending on how hard you are on your teeth and how well you maintain them. This is normal wear and tear, not a failure. Replacing the crown is straightforward—the implant and abutment usually stay in place.
If you've got implant-supported dentures, care depends on whether they're fixed or removable. Fixed versions get brushed and flossed just like individual implants—you're cleaning around the abutments where they come through your gums. Removable versions come out for cleaning like traditional dentures, but you also need to clean the abutments and the area around your implants.
The Economics of Dental Care: Thinking Long-Term
Let's talk money because it affects every decision about dentalcare. The cheapest option right now isn't always the cheapest option over time, and understanding the economics helps you make better choices.
Prevention is absurdly cost-effective. A tube of toothpaste costs a few bucks and lasts months. Dental floss is maybe five dollars. A decent electric toothbrush is $30-$100 and lasts years. Your six-month cleaning and checkup runs $75-$200 without insurance, much less with it. For maybe $300-$500 a year, you can prevent problems that cost thousands to fix.
A filling costs $150-$400. That same tooth, if the cavity grows, needs a root canal ($700-$1,500) and a crown ($800-$1,500). If it's too far gone, you're looking at extraction ($75-$300) and then replacement. Suddenly that $150 filling you skipped has cost you $3,000-$6,000 for an implant, or you're living with a gap, or you're getting a bridge that requires grinding down adjacent teeth.
Traditional dentures look cheap initially—$1,000-$3,000 per arch. But they need adjustment, relines, and replacement every five to eight years. Over twenty years, you're buying dentures three times, plus all those adjustments in between. Call it $7,000-$12,000, plus the cost of adhesives, cleaning supplies, and all the hassle.
Dental implants cost $3,000-$6,000 per tooth upfront. That's a lot. But over twenty-five years, you might replace the crown once ($1,000-$2,000). Total cost: $4,000-$8,000 for twenty-five years of service. The per-year cost isn't that different from dentures when you calculate it out, and you're getting significantly better function and bone preservation.
Implant-supported dentures at $15,000-$35,000 per arch seem expensive until you consider that they typically last fifteen to twenty-five years with minimal maintenance beyond normal dental care. No relining, no constant adjustments, no replacement dentures. The upfront investment is significant, but the long-term value often beats both traditional dentures and full implant restoration.
Insurance complicates the math. Most dental insurance covers preventive care (cleanings, exams) at 100%, basic procedures (fillings) at 80%, and major procedures (crowns, bridges) at 50%. Annual maximums typically cap at $1,000-$2,000, which doesn't go far when you need extensive work. Implants are often considered cosmetic and not covered at all, though this is gradually changing.
Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) let you pay for dental work with pre-tax dollars, which effectively gives you a discount equal to your tax rate. If you're paying 25% in taxes, that $4,000 implant only costs you $3,000 in after-tax dollars. Take advantage of these accounts if your employer offers them.
Many dental offices offer payment plans or work with healthcare credit companies like CareCredit. These often include interest-free periods if you pay the balance within a specified time. Read the terms carefully—if you don't pay it off in time, the interest rates can be brutal. But managed responsibly, they make expensive procedures accessible.
The hidden costs of poor dental health are harder to quantify but real. Missing work because of dental pain or infections. Limiting your diet because you can't chew properly, which can lead to nutritional deficiencies and other health problems. Avoiding social situations or career opportunities because you're self-conscious about your teeth. These have economic impacts that don't show up on a dental bill.
Special Situations: When Things Get Complicated
Some scenarios add complexity to dental care and tooth replacement decisions. Understanding these helps you navigate them if they apply to you.
Gum disease: This is the elephant in the room for tooth loss and implant success. You can't place implants in unhealthy gums—the infection will cause implant failure. Active periodontal disease needs treatment first: deep cleanings, antibiotics, possibly gum surgery. Once your gums are healthy, you can move forward with implants. Dentures are an option even with gum disease, but addressing the disease improves comfort and outcomes.
Diabetes: If you're diabetic, your dental care needs extra attention. High blood sugar impairs healing and increases infection risk. This affects everything from how quickly cavities develop to whether implants will integrate successfully. The good news is that well-controlled diabetes doesn't preclude implants—you just need your blood sugar stable, and your dentist and medical doctor need to coordinate care.
Osteoporosis and bone medications: Some medications for osteoporosis (bisphosphonates) can complicate dental procedures, especially extractions and implants. They affect how bone heals. If you're on these medications, your dentist needs to know before planning any surgery. This doesn't necessarily mean you can't get implants, but it requires careful planning and possibly consultation with your medical doctor.
Radiation therapy: If you've had radiation treatment to your head or neck for cancer, your bones and tissues in that area are compromised. Implant failure rates are higher, and healing is slower. Some people can still get implants, but it requires specialized care and careful evaluation. Dentures might be the more practical option depending on your specific situation.
Smoking: We've mentioned this repeatedly because it's that important. Smoking reduces blood flow to your gums, slows healing, increases infection risk, and dramatically raises implant failure rates. Most dentists require patients to quit (or at least significantly reduce) before placing implants. Even with dentures, smoking contributes to gum disease and bone loss.
Teeth grinding (bruxism): If you grind your teeth, you'll destroy crowns, crack implants, and damage dentures. A night guard is non-negotiable. It's a custom-fitted piece that protects your teeth (natural or artificial) while you sleep. Costs a few hundred bucks, lasts years, and prevents thousands in damage.
Limited mouth opening: Some people have TMJ issues or other conditions that limit how wide they can open their mouth. This makes dental work challenging—extractions, implant placement, even taking proper impressions for dentures becomes difficult. Discuss this with your dentist upfront so they can plan appropriately.
Multiple missing teeth with complex patterns: When you're missing teeth in various locations, treatment planning gets complicated. Individual implants for every gap might not make sense financially or logistically. Implant-supported bridges, partial dentures, or a combination approach might work better. This is where you really need an experienced dentist who can evaluate your whole situation rather than just treating one tooth at a time.
Making Decisions: A Framework That Actually Helps
You've got all this information now, but how do you actually make a decision? Here's a framework that helps people think through their options systematically.
Step 1: Assess your current situation honestly.
- How many teeth are you missing or failing?
- How's your overall oral health?
- Do you have any medical conditions that affect your options?
- What's your budget realistically, not what you wish it was?
- How do you feel about surgery?
Step 2: Identify your priorities. What matters most to you? Rank these:
- Appearance
- Function (ability to eat normally)
- Longevity
- Cost
- Avoiding surgery
- Convenience
- Bone preservation
There's no right answer, but knowing your priorities helps you weigh trade-offs. If function and longevity matter most and cost is secondary, implants probably win. If cost is primary and you're okay with some limitations, traditional dentures might be your answer.
Step 3: Consult with professionals. See at least two dentists who offer different solutions. Get opinions from:
- A prosthodontist (specialist in tooth replacement)
- A periodontist or oral surgeon (if considering implants)
- Your general dentist who knows your dental history
Compare their recommendations. If everyone suggests the same thing, that's probably your answer. If opinions differ, understand why—there might be multiple valid approaches to your situation.
Step 4: Consider the timeline.
- How quickly do you need a solution?
- Can you handle a multi-month process?
- Do you have upcoming events (wedding, job interview) where you need your teeth looking good?
Traditional dentures deliver faster. Implants take months. Factor this into your decision.
Step 5: Think long-term. Where will you be in five years? Ten? Twenty? Which solution serves you best not just now but over time? Sometimes the harder path initially (surgery, cost) leads to a better long-term outcome.
Step 6: Trust your gut. If something feels wrong about a particular dentist or approach, listen to that feeling. You need to be comfortable with both your dentist and your treatment plan. This is a significant commitment of time, money, and trust.
Living Well with Whatever You Choose
Here's the truth: there's no perfect solution that works for everyone. Traditional dentures work great for some people and are frustrating for others. Implants are life-changing for most but don't make sense for everyone. The goal is finding the right solution for YOU—your situation, your priorities, your life.
Whatever you end up with, commit to taking care of it. Good dentalcare isn't optional just because you've got dentures or implants instead of natural teeth. Your gums, your remaining teeth, your bone, your overall oral health—they all still matter. They affect not just your mouth but your general health, your quality of life, and your ability to eat, speak, and smile confidently.
Don't let perfect be the enemy of good. Maybe implants are the "best" solution technically, but if you can't afford them or don't qualify medically, well-maintained dentures are infinitely better than no teeth or teeth that are failing. Maybe traditional dentures seem old-fashioned, but if they work for you and you're happy with them, that's what matters.
Stay engaged with your dental health. See your dentist regularly. Ask questions when something doesn't feel right. Keep learning—dental technology evolves, and options that weren't available five years ago might be perfect for you now.
And remember: your teeth affect way more than just your mouth. They influence what you eat, how you speak, how you feel about yourself, how you interact with other people. Taking care of them—whether they're natural, attached to implants, or removable—is taking care of yourself. That's always worth the effort.
The path you choose doesn't have to be the path someone else would choose. It just has to be the right path for you, based on your circumstances, your goals, and your honest assessment of what you're willing and able to commit to. Make that decision from a place of understanding rather than fear or confusion, and you'll be fine.
Your smile matters. How you get there—dentures, implants, or something in between—is less important than ending up with a solution you feel good about and can maintain for the long haul. Take your time, ask your questions, and make the choice that lets you live fully and confidently. You deserve that.
